IBS pain relief: 9 Most Effective Tips From A Doctor With IBS.
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Get ready because I’m about to unpack a goldmine of insights about IBS pain relief techniques.
These aren’t just any techniques; they’ve allowed me to keep my IBS attacks at bay 90% of the time.
Think of this as your comprehensive guide. It’s an intimate fusion of my disease experience with solid, research-backed data straight from the trenches of a gut doctor with IBS.
Moreover, this guide stands on a firm evidence-based foundation so that you can set realistic expectations. It’s your reliable beacon amidst the flood of misinformation that’s out there on the internet.
Now, let’s get specific. I’ve honed in exclusively on IBS pain relief for this guide. But worry not; in-depth guides on tackling IBS diarrhea, constipation, bloating, and gas are coming soon.
To make this guide digestible, I’ve split it into two main sections:
- Section 1: Immediate IBS pain relief tips you can implement RIGHT NOW.
- Section 2: Strategic advice for long-term pain relief you can initiate today for payoffs in the future.
Let’s dive into it. But before that, here is a table summary of the best IBS pain relief tips:
| Tip | Description |
|---|---|
| 1. Listen to Your Colon | Avoid suppressing the urge to go to the restroom, as this can exacerbate IBS symptoms. Regular colon evacuation can relieve mild IBS flare-ups. |
| 2. Use Heat | Heat relaxes the muscles in the colon, reducing pain and bloating. Use a safe, high-quality heating pad on painful areas. |
| 3. Try Antispasmodics | Prescription and over-the-counter antispasmodics can help to alleviate IBS pain. Always stick to the recommended dosage and consult your healthcare provider. |
| 4. Herbal Teas | Certain herbal teas, such as peppermint tea, can help relieve IBS pain. However, overconsumption can exacerbate IBS or cause heartburn. |
| 5. Eliminate Trigger Foods | Certain foods, especially those high in FODMAPs, can trigger IBS pain. Consider eliminating lactose and gluten, and reduce insoluble fibers and grassy foods. |
| 6. Understand Mind & IBS Connection | Stress and anxiety can trigger IBS flare-ups. Manage your thoughts to help relieve your IBS pain. Techniques like cognitive-behavioral therapy can help. |
| 7. Try an Elimination Diet Plan | Identifying and eliminating trigger foods can significantly relieve IBS symptoms. |
| 8. Embrace Probiotics | Probiotics help to restore balance in the gut, which can reduce IBS symptoms. |
| 9. Practice Physical Activity | Regular physical activity can reduce IBS symptoms by decreasing anxiety and depression and improving gut motility. |
Section 1: Short-term IBS Pain Relief Tips.
1- Listen To Your Colon.
At its core, this is a remarkably straightforward yet potent IBS pain relief strategy.
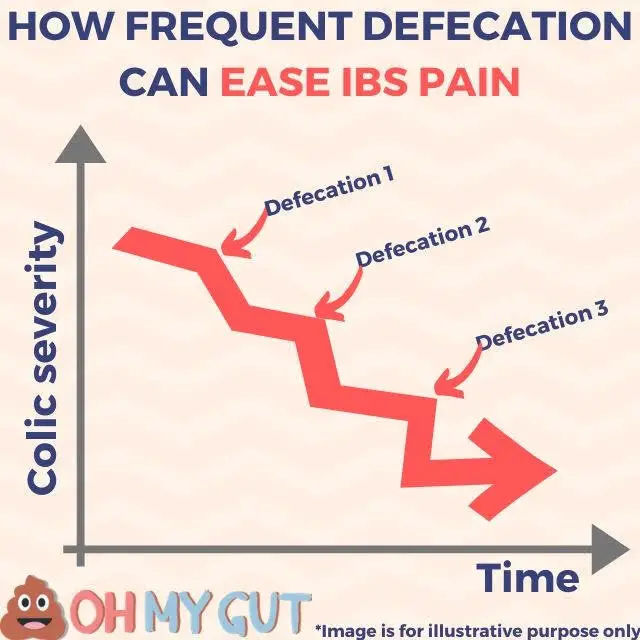
In the simplest terms, IBS is characterized as “abdominal pain associated with defecation.” The “association” implies that, for most people, abdominal discomfort improves with bowel movements (though a small fraction may experience worsening symptoms after defecation).
Essentially, your abdominal pain is your body’s way of communicating with you, urging you to “empty” your colon.
I’ve consistently managed to dispel mild IBS flare-ups solely by ensuring regular colon evacuation. The good news? It works over 90% of the time, usually bypassing the need for antispasmodics altogether.
NOTE: this is not a very effective method in people with IBS constipation.
Heading to the restroom every 10 minutes. Generally, my IBS symptoms start to subside after about 4 to 5 frequent trips.
So, the first step in your IBS pain relief journey is to heed this signal. Never restrain yourself from visiting the restroom; it may only exacerbate your IBS symptoms.
In my observation, those who tend to suppress the urge for a toilet visit suffer the most from IBS. You might be more prone to this in situations like:
- Anxiety about using the restroom at work or school.
- Nervousness about needing the restroom at outdoor social events like visits or parties.
- Fear of using the restroom during long trips, such as on trains or airplanes.
Training yourself to overcome any overthinking or embarrassment related to using public restrooms is crucial.
By suppressing the urge to visit the toilet, all you’re doing is prolonging your discomfort and intensifying the colic.
Is there scientific evidence for this?
Of course, the evidence about this technique lies in the definition and diagnostic criteria for IBS itself. According to Rome IV criteria, The IBS abdominal pain is related to defecation (bowel movements). And more than 95% of the time, the pain is relieved by defecation (reference).
However, in a minority of IBS patients, defecation may worsen the pain (rather than relieving it).
2- Use heat to relieve IBS abdominal pain.
Heat therapy is one of the simplest and most effective ways to alleviate pain; IBS-related abdominal discomfort is no exception.
Here’s why heat can be so effective:
The root cause of IBS pain is the contractions of the muscles in your colon wall. Irregular or intense contractions result in pain and bloating and may lead to diarrhea.
Applying heat relaxes these muscles and reduces colics. It’s a cost-effective and safe remedy for IBS pain relief for most people.
Here’s how to leverage it effectively:
- Use it as an adjunct to the other tips listed here, but keep expectations in check.
- Always use safe, high-quality heating pads with automatic shut-off to prevent burns.
- Apply heat to the most painful area. Like this one on Amazon (Amazon affiliate link), a heating pad is usually your best bet.
- NEVER apply heat pads directly to your skin. Always put a layer or two of cloth between your skin and the heat source.
- Use it for at least 15 minutes, but don’t exceed 2 hours.
- Try to relax in a comfortable position and perhaps listen to soothing music.
- Never fall asleep with the heating pad on your stomach.
3- Try Antispasmodics.
The most straightforward way to alleviate IBS pain is by using antispasmodics. You have two main categories to choose from:
Prescription antispasmodics: For example, mebeverine hydrochloride (ColofacⓇ) and tricyclic antidepressants like amitriptyline have antispasmodic effects.
Over-the-counter antispasmodics: The most popular ones include peppermint oil (IBgard) (Amazon affiliate link).
Both prescription and over-the-counter antispasmodics have proven effective in alleviating IBS pain.
If you decide to use antispasmodics, here are some pointers:
- Start with over-the-counter options; they’re generally safer and have fewer side effects. IBgard (Amazon affiliate link) is the only available OTC antispasmodic in the USA.
- Stick to the recommended dosage for the antispasmodics. Don’t let the pain lead you to misuse these medications.
- For the best effect, take the antispasmodic 15 minutes before meals.
- Enhance results by avoiding foods that trigger IBS and large meals.
- Always consult your healthcare provider about the duration, potential side effects, and any contraindications specific to your health condition.
If you plan to use antispasmodics, check out this guide that tells you exactly how to use them for IBS pain relief.
4- Herbal Teas Can Also Help.
A warm cup of herbal tea can also aid IBS pain relief. Teas specific to IBS, like peppermint oil tea, can be particularly effective.
Peppermint tea, for example, can relieve IBS pain like peppermint oil capsules.
Try Organic Peppermint Tea (Amazon affiliate link).
Please note: Overconsumption of herbal teas might exacerbate your IBS or cause heartburn. Also, remember that these herbal teas haven’t been thoroughly studied. Results can vary, but they’re worth a shot.
5- Eliminate Foods That Aggravate Your IBS.
Certain foods are known to trigger IBS pain. Eliminating these during an IBS attack is one of the most effective strategies to mitigate pain.
These include:
A. Gas-producing foods: such as beans, onions, celery, carrots, raisins, bananas, apricots, prunes, Brussels sprouts, wheat germ, pretzels, bagels, alcohol (especially high FODMAP alcohols), and caffeine.
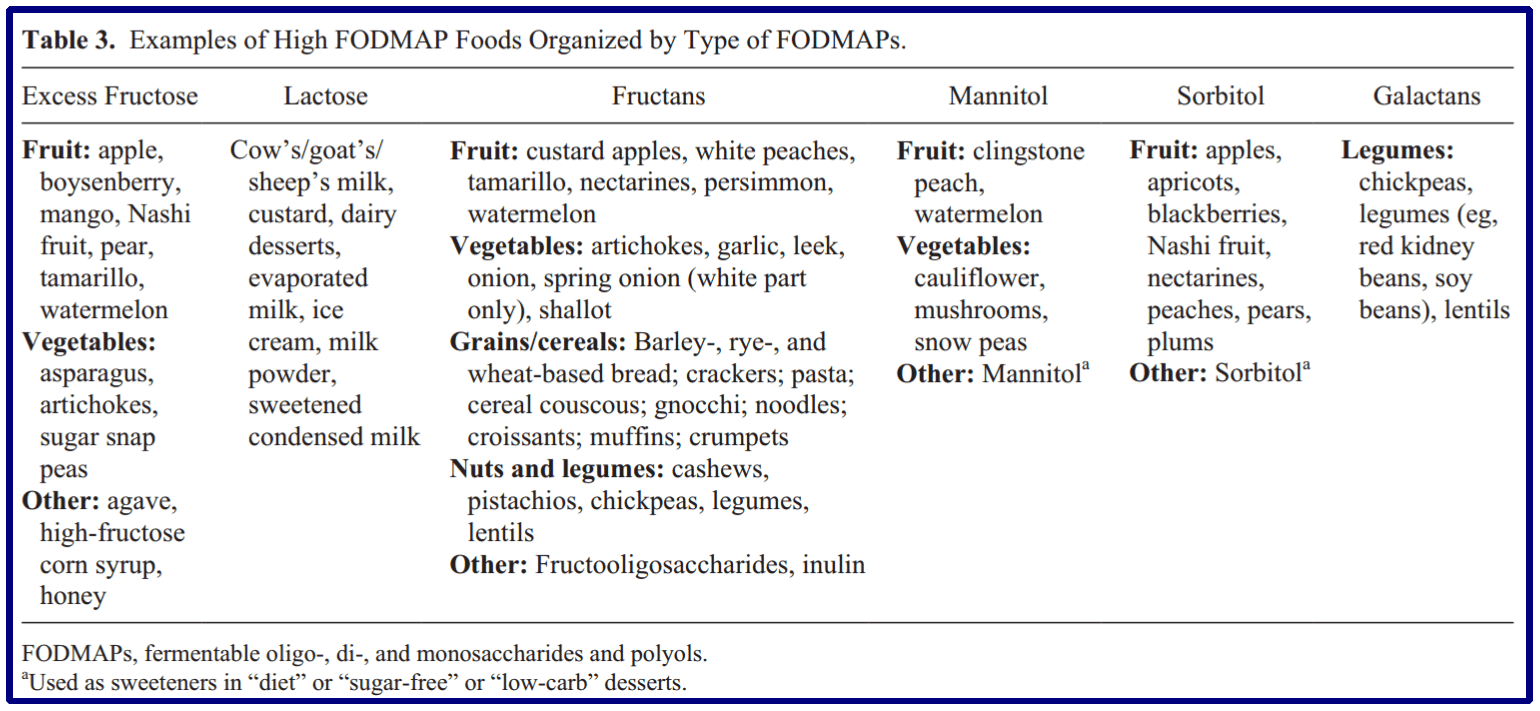
B. Foods high in FODMAPs: These foods are known to trigger IBS pain. They are types of sugars that are easily fermentable and produce a lot of gas, including:
Fermentable foods, as gut bacteria break them down, produce excess gas. Oligosaccharides: fructans and galacto-saccharides are present in wheat, barley, rye, onion, garlic, and legumes. Disaccharides: lactose sugar present in milk, ice cream, custard, and yogurt. Monosaccharides: Free fructose is present in apples, pears, mangoes, cherries, watermelon, asparagus, sugar snap peas, honey, and high-fructose corn syrup. Polyols: sorbitol, mannitol, xylitol, and maltitol are present in certain fruits like apples and watermelon and in artificial sweeteners like artificially sweetened gum and alcohol.
The image below illustrates common foods high in FODMAP content triggering IBS (reference).
Instead, you can try foods low in FODMAP content; see the image below (reference).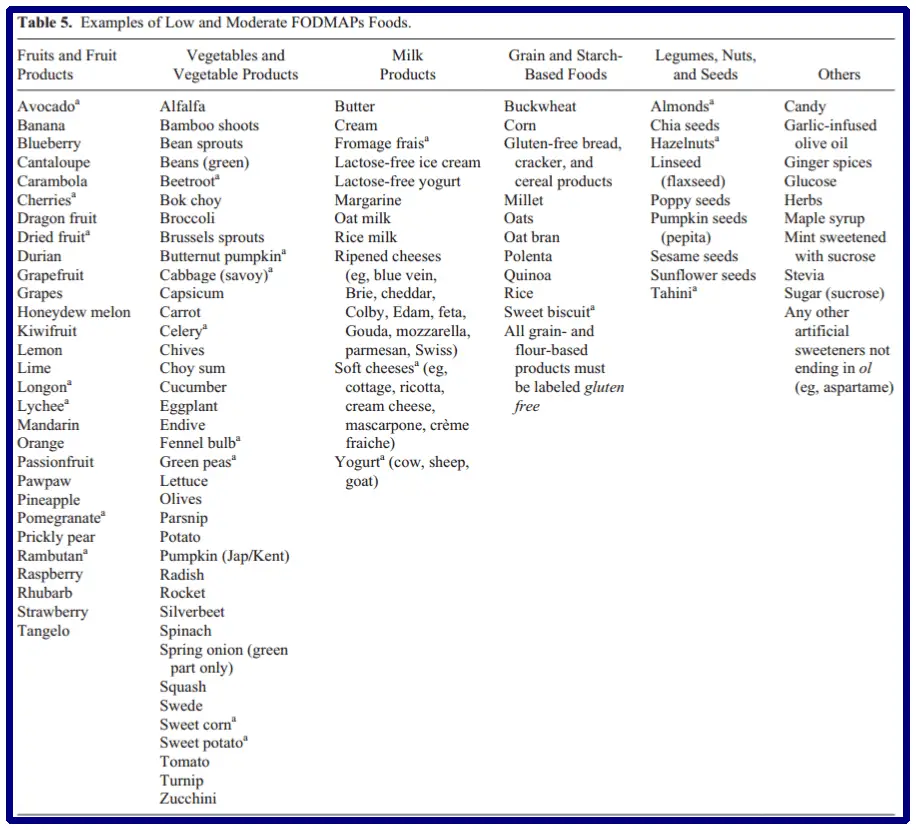
C. Consider eliminating lactose and gluten:
If you’ve tried the above steps without success, you may want to consider cutting lactose (in milk, ice cream, and other dairy products) and gluten (in wheat and barley).
Some studies suggest that many people with IBS benefit from excluding these two foods. This doesn’t mean you have lactose intolerance or celiac disease (gluten intolerance), but mild degrees of sensitivity could exist in IBS. Again, the response to cutting out these foods varies from person to person.
If you need guidance on properly eliminating these foods from your diet, look at the diet elimination plan below.
D. Reduce insoluble fibers and grassy foods:
There are two types of fibers, soluble and insoluble. Both can either help or harm your IBS.
Insoluble fibers: found in grassy foods, cabbage, broccoli, and fruits. They don’t dissolve in water. If you consume too much insoluble fiber, it can cause IBS pain, bloating, and gas. Soluble fiber: dissolves in water and, when consumed in the right amount, can help manage your IBS. They’re particularly effective in IBS diarrhea as they trap water and form a gel. They’re found in whole grains like brown rice and some fruits.
[part 2] Long-term IBS pain relief strategies:
6- A Mindful Beginning: Understanding the Connection between Your Mind & IBS
It’s surprising how significantly our mind impacts our physical health, specifically conditions like IBS. Regardless of source stress and anxiety have been linked to IBS flare-ups.
According to research, people with IBS often have higher levels of:
- Anxiety
- Depression
- Phobias
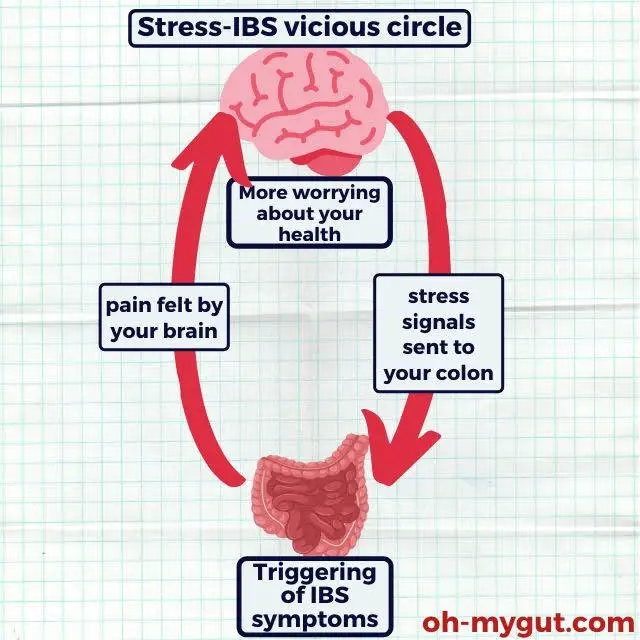
Anxiety, our body’s response to stress and apprehension, is one of the most common issues I see in my patients. It refers to the sense of fear or uncertainty about future events. Ironically, one of the most recurring causes of IBS flare-ups is the worry about IBS itself.
Many IBS patients fret about their conditions, thinking it’s a severe disease or, worse, confusing it with conditions like colon cancer. This state of anxiety only exacerbates IBS symptoms, forming a vicious cycle:
More fear & thinking > more stress signals from your brain to your colon > IBS pain > your brain detects pain from your colon > More fear and thinking.
Other external factors, such as financial stress or uncertainty in personal relationships, can trigger IBS symptoms. The impact on your health is multi-faceted, causing:
- Triggering of IBS pain, diarrhea (more commonly), or constipation.
- Sleep disorders.
- Rapid heartbeat.
- Chronic stress and headache.
Therefore, understanding and managing your thoughts is the first step to relieving your IBS pain.
Here are some handy tips for managing anxiety:
1- Identify & Dismiss Your “Destructive Thoughts”
Understanding your thought process is crucial. Ask yourself, what are you worrying about? What are your expectations of future events?
For instance, a 42-year-old patient of mine suffered frequent IBS attacks due to his fear of colon cancer (his close friend, aged 47, had colon cancer). He constantly worried that his abdominal aches might indicate colon cancer – an unwarranted fear causing him chronic stress and recurrent IBS flare-ups.
Once he understood the baselessness of his thoughts, he saw improvement. This self-reflection and cognitive restructuring process is called “Cognitive-Behavioral Therapy” (CBT) for IBS.
Source: this study
2- Say Goodbye to Expecting the “Worst Scenario”:
Once you’ve identified those naughty thoughts, it’s time to put them under the microscope and RE-LABEL them. Here’s the issue with your anxiety – it’s a bit like a movie director who only films disaster scenes. But let me tell you something. As every movie isn’t a catastrophe, IBS isn’t your worst-case scenario. It’s a benign condition that won’t take you through dangerous complications.
Pro tip:
Want to nail this thought identification and re-labeling process? Get it down on paper. Nothing sorts out thoughts like writing them out.
3- Let Your Stress See the Light of Day!
Now, let’s talk about your anxiety. Yes, literally! Start by sharing your fears and worries with your partner or a close family member. You’ll be amazed at how much clarity comes from simply expressing your thoughts aloud. Your fears and illogical expectations’ll start looking much less scary once you’ve spoken about them.
If you want to up the ante, consider consulting your gastroenterologist. They can guide you to CBT or an online CBT platform like online-therapy.com. This service specializes in Cognitive Behavioural Therapy with many tools and resources. Online CBT has been shown to have the same effect as face-to-face CBT. Even the American Psychological Association has endorsed guidelines for Online CBT (telepsychology).
7- Master an Elimination Diet Plan like a Pro.
Imagine being a food detective to manage your IBS – sounds exciting, right? I consider eliminating trigger foods one of the most rewarding strategies to control your IBS. (Evidence 1) (Evidence 2)
Here’s why embarking on an elimination diet plan can be a game-changer:
- Sniffs out and eliminates food triggers.
- It can significantly relieve IBS pain and bloating.
- A safe, affordable strategy to take charge of your IBS.
- It can be self-managed if you’re up for the challenge.
8- Embrace Probiotics.
Ever considered how probiotics work? (reference1 | referece2 | reference3)
Your gut is like a bustling city, teeming with bacteria. You provide them with shelter and food; in return, they help your gut digest food and keep unwanted guests (like harmful bacteria) at bay.
But in IBS, the balance of power between the good bacteria (your allies) and the bad ones (the invaders) can get disrupted. This imbalance can trigger classic IBS symptoms like abdominal pain, bloating, diarrhea, or constipation.
That’s where probiotic supplements, AKA “good bacteria,” come to the rescue. They can help restore balance and harmony in your gut city.
If you want to get started right away, here’s my top pick for a probiotic (packed with strains that specifically help with IBS from a reputable manufacturer with loads of positive reviews on Amazon and other platforms):
Top-rated Probiotic on Amazon.com
9- Movement and Exercise.
Physical activity is essential for IBS pain relief. Regular movement and exercise can help in several ways:
- It can reduce your stress levels, which may help reduce IBS symptoms.
- It can help to normalize bowel movements and prevent constipation.
- It helps to increase overall well-being and quality of life.
While it’s not necessary to become a gym addict, moderate, regular physical activity like walking, yoga, cycling, or swimming can provide relief. A study demonstrates how regular physical activity can improve IBS symptoms.
- Evidence-based
- Written by a doctor.

Related Posts:
- Does Ibuprofen trigger or relief IBS? GI doctor Explains
- How To Cure IBS In One Day (9 most effective strategies)
- Anxiety & IBS: Roots & Practical tips to…
- Magnesium For IBS: In-depth Doctor's Review.
- IBS in pregnancy: Risks & Best treatments (GI Doctor…
- How To Diagnose IBS (Simplified + Quiz), Doctor Explains.






