Does Ibuprofen trigger or relief IBS? GI doctor Explains
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Are you grappling with the discomfort of Irritable Bowel Syndrome (IBS) and wondering if that handy bottle of Ibuprofen in your medicine cabinet is a friend or foe?
You’re not alone.
Many people with IBS find themselves in this conundrum, unsure if this common pain reliever will ease their symptoms or send them running for the nearest restroom.
In this article, we’re going to delve into the complex relationship between Ibuprofen and IBS, shedding light on whether this popular medication is a trigger or a helper when it comes to managing this often unpredictable condition.
So, buckle up and get ready for a deep dive into the world of IBS and Ibuprofen!
Key Facts:
- There’s no evidence to support the use of NSAIDs for IBS pain relief.
- When managing pain, consider ibuprofen and Paracetamol relatively safer options than other NSAIDs like ketoprofen or aspirin.
- Using ibuprofen and certain NSAIDs might worsen your IBS symptoms.
- Always consult your doctor to determine the safest treatment options for your IBS.
- Avoid using opioid analgesics for IBS pain relief.
1- Can Ibuprofen Be Used for IBS Pain Relief?
In a nutshell, no.
Ibuprofen doesn’t help with IBS pain. According to the Rome IV criteria for diagnosing and managing IBS, there’s no recommendation for using ibuprofen in treating IBS.
Why? Because IBS pain isn’t inflammatory. It’s caused by spasms in the smooth muscles in the wall of your colon, as explained here. These spasms don’t respond to painkillers like ibuprofen. Instead, they respond to antispasmodics like anticholinergic drugs, peppermint oil, or mebeverine.
However, some patients report IBS relief with ibuprofen. This is an exception rather than the rule, and a variety of factors can explain it:
1- Overlap of IBS pain with other chronic pain syndromes like fibromyalgia: This association is uncommon. People with fibromyalgia experience widespread muscle and joint pain. (Reference)
If you have fibromyalgia-associated IBS, your gut pain may respond to ibuprofen. Discuss this with your doctor, especially if you have generalized muscle aches or headaches.
You can read more about fibromyalgia and IBS here.
2- Overlap of IBS pain with menstrual pain in females: Period pain can be confused with IBS. If you’re a female and experience abdominal pain before or during menstruation, this can be confused with IBS pain.
3- Overlap between IBS pain and any other inflammations inside your abdomen: Conditions like cholecystitis, renal pain, and appendicitis can be confused with IBS pain. These inflammatory conditions may respond to ibuprofen.
So, if you experience improvement in your IBS symptoms with ibuprofen, it may mean that you have other conditions associated with your IBS. Always consult your doctor in such cases.
2- Can Ibuprofen trigger IBS making it worse?
Ibuprofen can potentially worsen your IBS. It’s generally safer to use Paracetamol (acetaminophen) instead, which is relatively safer than ibuprofen. Ibuprofen can cause side effects, especially when overused without medical supervision.
The side effects of ibuprofen can exacerbate your IBS symptoms. They include:
- Abdominal pain (over your stomach or all over your abdomen).
- Potential diarrhea.
- Increased gas and bloating.
- Nausea and vomiting.
Moreover, Non-steroidal anti-inflammatory drugs (NSAIDs) can affect your intestine and colon even if you don’t have IBS. This study illustrates the possible complications of NSAIDs (including ibuprofen) affecting your lower gastrointestinal tract (small intestine and colon):
- Malabsorption of fluids and nutrients.
- Induction of gut inflammation.
- Increased gut permeability to toxins and bacteria passing into your bloodstream.
- This may lead to ulcers in the mucosa of your intestine.
- These ulcers or erosions may lead to blood loss and anemia.
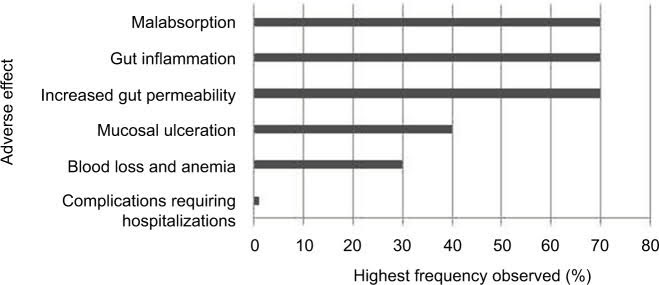
Source: This study
In addition to impacting IBS, Ibuprofen may also lead to other serious complications, such as:
- Increasing the risk of gastritis (inflammation of your stomach lining).
- Potentially causing stomach or duodenal ulcers.
- Possibly leading to heart problems.
- Potentially affecting kidney function.
So, it’s crucial not to use ibuprofen if you have IBS unless your healthcare provider prescribes it.
Ibuprofen can potentially trigger IBS attacks. If you notice IBS symptoms after taking ibuprofen, you should stop taking it and consult your doctor immediately.
4- Ibuprofen Gel and IBS
Ibuprofen gel is commonly used to treat various painful conditions, excluding abdominal pain. Typical uses of Ibuprofen gel include:
- Joint pain such as knee osteoarthritis.
- Backache.
- Muscle pain.
- Pain from strains and sprains.
There’s no evidence to suggest that applying Ibuprofen gel to your abdomen can alleviate your IBS symptoms. Ibuprofen gel is primarily used for muscular pain, arthritis, backache, and pain from strain and sprains.
Conversely, only minimal amounts of ibuprofen gel pass into your bloodstream. So, using ibuprofen gel for joint or muscle pain is unlikely to exacerbate your IBS.
Remember, Ibuprofen gel should only be applied to intact skin. Never attempt to apply ibuprofen gel to the anal area or lips (it’s for external use only).
5- Can I Take Ibuprofen If I Have IBS?
While using ibuprofen to treat your painful conditions and headaches is not contraindicated if you have IBS, it’s always best to consult your doctor. Ibuprofen has the potential to worsen your IBS symptoms.
As previously mentioned, it may increase abdominal pain, gas, and bloating and cause constipation. If you plan to use ibuprofen for any reason (fever, headache, muscle or joint pain), proceed with caution or consider safer alternatives.
Tips to safely take ibuprofen with IBS:
Here are some tips for safely using ibuprofen with IBS:
- Talk to your doctor before taking ibuprofen. Even though ibuprofen is available over-the-counter, it’s still a drug and can have side effects. Your doctor can help you decide if ibuprofen is right for you and can help you find a safe dosage.
- Try other pain relievers first. Other pain relievers, such as acetaminophen (Tylenol) or naproxen (Aleve), are less likely to worsen IBS symptoms. If you can, try these before using ibuprofen.
- Start with a low dose. The lowest effective dose is usually the best option, especially if you have IBS. Start with 200 mg of ibuprofen and see how you feel. Take another 200 mg after 4-6 hours if you need more pain relief.
- Take ibuprofen with food. This will help to slow down the absorption of ibuprofen and reduce the risk of stomach upset.
- Don’t take ibuprofen for more than ten days. Long-term use of ibuprofen can increase your risk of side effects, such as stomach ulcers.
- Stop taking ibuprofen if your IBS symptoms get worse. If you notice your IBS symptoms worsening after taking ibuprofen, stop taking it and talk to your doctor.
If you have IBS and need pain relief, talking to your doctor about the safest way to take ibuprofen is important. They can help you find a pain reliever that’s right for you and won’t worsen your IBS symptoms.
Pro Tip: If you need ibuprofen, use the gel instead of oral tablets. The gel form is absorbed more slowly into your bloodstream, which can help to reduce the risk of stomach upset.
6- Tylenol and other NSAIDs with IBS.
There are several NSAIDs available, most of which require a prescription. However, one exception is acetaminophen, commonly known as Paracetamol, which you can find over-the-counter. It’s an anti-inflammatory drug and is generally considered safer than ibuprofen.
When managing your IBS and taking care of your stomach, acetaminophen and ibuprofen cause fewer side effects compared to other NSAIDs like Ketoprofen, Meloxicam, and aspirin.
Paracetamol (acetaminophen) is particularly gentle on your IBS and stomach, and it’s also considered safe for your kidneys and heart.
It’s important to note that no evidence supports the idea that NSAIDs can help with your IBS pain. So, keep that in mind.
For pain management, ibuprofen and Paracetamol are generally safer than other NSAIDs like ketoprofen or aspirin.
Using ibuprofen and other NSAIDs may worsen your IBS symptoms, so it’s better to be cautious.
Remember, working closely with your doctor to figure out the safest options for managing your IBS is always best.
Oh, and one last thing – avoid using opioid analgesics for IBS pain, as they may not be beneficial in the long run.
FAQs about IBS and ibuprofen.
Is Ibuprofen bad for IBS?
Like other non-steroidal anti-inflammatory drugs (NSAIDs), Ibuprofen can potentially worsen IBS symptoms in some people. These medications can irritate the gut’s lining and affect its function, leading to symptoms like abdominal pain, diarrhea, or constipation. However, everyone is different, and some people with IBS may not experience any adverse effects from ibuprofen. It’s always best to consult your healthcare provider before starting any new medication.
Can I take ibuprofen for IBS pain?
While ibuprofen can help with general pain relief, it’s not typically the first choice for managing IBS pain due to its potential to irritate the gut. Other treatments, such as antispasmodics, peppermint oil, and certain types of antidepressants, are often recommended first. However, if you’re considering taking ibuprofen for IBS pain, discussing this with your healthcare provider to weigh the potential benefits and risks is important.
Does ibuprofen cause constipation with IBS?
Ibuprofen doesn’t typically cause constipation but can affect each person differently. In some people with IBS, particularly those with IBS-C (constipation-predominant IBS), ibuprofen may worsen constipation by affecting gut function. If you have IBS and need to take ibuprofen or any other medication, it’s always best to consult your healthcare provider to understand the potential effects on your condition.
- Evidence-based
- Written by a doctor.

Related Posts:
- IBS pain relief: 8 Most Effective Tips From A Doctor…
- How To Diagnose IBS (Simplified + Quiz), Doctor Explains.
- IBS in pregnancy: Risks & Best treatments (GI Doctor…
- Magnesium For IBS: In-depth Doctor's Review.
- IBS or Colon Cancer: In-depth Guide to Differences…
- Does Pepsi Help with Nausea? (GI Doctor Explains)





