Constant Diarrhea: 8 Common Causes (Gastroenterologist Explains).
Our content is not intended nor recommended as a substitute for medical advice by your doctor. Use for informational purposes only.
Let’s define things; what is constant diarrhea?
Diarrhea is the passage of 3 or more loose or liquid stools per day. This is the official definition of the WHO organization.
Frequent passage of well-formed stool (more than three times daily) is not considered diarrhea.
Constant diarrhea is not an “official” medical term we use as doctors. We classify diarrhea into three major categories (reference):
- Acute diarrhea: Any diarrhea that lasts less than two weeks (14 days).
- Persistent diarrhea: more than 14 days, but fewer than 30 days.
- Chronic diarrhea: More than 30 days in duration.
Constant diarrhea lasting for more than one month is considered chronic diarrhea. Some people also may refer to persistent diarrhea as constant diarrhea.
Also, some people refer to persistent diarrhea as a form of constant diarrhea.
Acute diarrhea is almost exclusively due to the infection of your intestines with pathogens (reference).
The causative organisms of acute infectious diarrhea are:
- Viruses (viral gastroenteritis or stomach flu) are the most common type of infection. Common viruses are Norovirus, Rotavirus, and Adenovirus.
- Also, bacteria, protozoa, and even fungi can cause acute diarrhea.
What Causes chronic or constant diarrhea?
In summary, the causes of chronic or constant diarrhea include (reference) the following:
The causes were arranged in the order of commonality (the common, the infrequent, and the rare causes of chronic or constant diarrhea.
| Frequency | Causes of chronic or constant diarrhea |
| 1- Common | 1. IBS-diarrhea 2. Bile acid diarrhea 3. Diet (Food Intolerance) 3. Colonic Tumors (Cancers and benign tumors) 4. Inflammatory bowel diseases 5. Celiac disease 6. Drugs 7. Recurrent Clostridioides (formerly Clostridium) difficile diarrhea 8. Overflow diarrhea |
| 2- Infrequent | 1. Small bowel bacterial overgrowth 2. Mesenteric ischemia 3. Lymphoma 4. Surgical causes (e.g., small bowel resections, fecal incontinence, internal fistula) 5. Chronic pancreatitis 6. Radiation enteropathy 7. Pancreatic carcinoma 8. Hyperthyroidism 9. Diabetes 10. Giardiasis (and other chronic infections) 11. Cystic fibrosis |
| 3- Rare | 1. Rare small intestinal diseases (e.g., Whipple’s disease, tropical sprue, amyloid, intestinal lymphangiectasia) 2. Hypoparathyroidism 3. Addison’s disease 4. Hormone-secreting tumors (VIPoma, gastrinoma, carcinoid) 5. Autonomic neuropathy 6. Factitious diarrhea 7. Brainerd diarrhea (possible infectious cause not identified) |
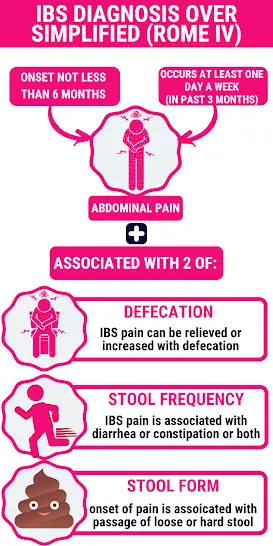
1- Irritable Bowel Syndrome with diarrhea.
Irritable bowel syndrome affects too many people worldwide. Approximately 10 to 15% of people have IBS (reference).
Surprisingly, Too many people who match the criteria of IBS don’t seek medical advice. Some studies estimated that 60% of people with IBS symptoms don’t know they have the disease! (reference).
IBS has four subtypes according to the predominant symptom. What concerns us today is the diarrhea-predominant IBS. Diarrhea-predominant IBS is one of the most common causes of constant diarrhea.
Symptoms (how to suspect IBS-diarrhea):
- Abdominal pain: is the fundamental symptom of IBS. IBS sufferers have experienced abdominal pain at least one day per week for the past three months.
- The abdominal pain either improves or worsens after the bowel movement.
- The onset of abdominal pain is associated with diarrhea and loose stool (change in stool form).
- Bloating is frequent in people with IBS.
- Intermittent or constant diarrhea.
- Mucus in the stool.
The IBS is usually triggered by:
- Certain foods, such as FODMAPs.
- Alcohol and caffeine.
- Fatty foods and spicy foods.
- Stress and anxiety.
The following symptoms are NOT among IBS symptoms:
- Abdominal pain awakens you at night.
- Fever.
- Blood in stool.
- Weight loss.
- Vomiting.
- Anemia.
IBS is a functional bowel disease. This means we couldn’t find specific lesions by investigation. IBS can only be diagnosed by a doctor after the exclusion of other organic diseases.
The ROME IV criteria are the most accepted method for diagnosing IBS. The ROME IV symptom-based criteria. Until now, No specific imaging or lab test can diagnose IBS.
If you suspect IBS is a cause of constant diarrhea. Learn how IBS is diagnosed in this in-depth article.
Arrange a visit to your doctor to get diagnosed.
2- Bile acid diarrhea.
Bile acid diarrhea (BAD) is one of medicine’s most underrated causes of chronic and constant diarrhea.
Normally, your small intestine reabsorbs more than 95% of bile excreted from the liver through the gallbladder and bile duct (reference).
Excess bile acid secretion or malabsorption of the bile acid leads to Bile acid diarrhea.
How common is bile acid diarrhea?
Bile acid diarrhea is more common than you think. And it is often misdiagnosed as IBS-D.
The following facts and statistics will help you imagine the amplitude of BAD:
- About 25 to 50% of patients diagnosed with IBS-diarrhea have BAD (reference).
- It is estimated that about 1% of the population may have BAD.
- It is estimated that about 64% of patients with Functional diarrhea have BAD (reference).
- Up to 35% of people with “microscopic colitis” condition have BAD (reference).
Symptoms suggest Bile acid diarrhea.
- Constant diarrhea (especially after fatty meals).
- Extreme urgency: a sudden severe urge to poop.
- Extreme urgency may lead to soiling accidents (stool incontinence) in some people.
- Unlike IBS, diarrhea can occur at night (it awakens you from sleep).
- Abdominal pain and stomach gurgling after meals.
- Bloating and flatulence.
Many doctors overlook bile acid. This is due to the relative unavailability of its specific test (SeHCAT test) and the similarity of symptoms with IBS.
The treatment of bile acid diarrhea is a bile acid binder called cholestyramine (Questran). We discussed the issue of BAD and its relation to IBS-D in-depth HERE.
3- Diet (a big cause of constant diarrhea).
Intolerance or allergy to certain foods or drinks is a widespread condition. It is estimated that up to 20% of people have some form of food intolerance.
Lactose is a sugar present in milk and other dairy products. Lactose intolerance is shockingly common among some races.
The prevalence of lactose intolerance in the white population is about 20%, which may increase to 90% in certain other races (reference).
Lactose intolerance is just one example of food intolerance. A long list of foods and drinks can cause food intolerance or allergy.
Common types of food intolerance and allergy:
- Lactose intolerance:
Present in milk, ice cream, mustard, and some types of cheese. - Fructose intolerance:
Present in many fruits and honey. - FODMAPs intolerance:
It affects people with IBS. FODMAPs refer to “Fermentable Oligo-, Di-, Monosaccharides, and Polyols. FODMAPs are a group of short-chain carbohydrates that cause gas and digestive disturbances. They are present in various foods, vegetables, fruits, and artificial sweeteners. Learn more. - Caffeine intolerance:
Caffeine in coffee, teas, and chocolates is one of the most common causes of constant diarrhea. Caffeine is usually abused in large amounts, raising diarrhea risk.
- Alcohol intolerance:
Much alcohol causes diarrhea, some of which are high in FODMAPs and can trigger IBS symptoms.
- Gluten intolerance:
It causes Celiac disease (see later) and another milder form called “Non-celiac gluten sensitivity.” - Amines intolerance:
Bacteria produce amines during food storage and fermentation. - Salicylates intolerance:
Salicylates are naturally occurring chemicals. They are present in various foods, including fruits, vegetables, coffee, and teas. - Sulfite intolerance:
Sulfite is used as a natural preservative for foods. - Food allergy:
Some foods can cause more severe allergic reactions, such as Nuts, peanuts, raw meat, seafood, mustard, rice, and some fruits and vegetables.
The difference between food intolerances and food allergies is described in the table below:
Food intolerance | Food allergy |
| Affects 15-20% of the population | Affects nearly 2-5% of adults |
| Difficulty digesting certain types of food (not immune-mediated allergy). | An immune-mediated reaction to certain foods or food components. |
| It can cause “constant” or “chronic” attacks of diarrhea. | Usually causes acute attacks or is related to the ingestion of offending food. |
| Intestinal symptoms: diarrhea, extensive gas, bloating, and abdominal pain | Intestinal symptoms are the same |
| No extra-intestinal symptoms | Extra-intestinal symptoms like rashes, urticaria, swollen lips or face, or severe life-threatening allergic reactions. |
| The severity of your symptoms is proportional to the amount you eat from the offending food. | Even trace amounts of the offending food can produce severe symptoms. |
Common offending foods:
| Common offending foods: (examples)
|
4- Celiac disease.
Celiac disease is an extreme form of food intolerance. It is a common disease affecting 1% of the world’s population.
With celiac disease, your body is intolerant to a protein called “gluten.” Gluten is found mainly in:
- Wheat and wheat-based foods such as bread.
- Rye.
- Barley.
A small intestinal inflammation with malabsorption develops after eating gluten-containing foods. Celiac disease can cause constant diarrhea for years if people don’t seek medical advice.
Symptoms suggesting celiac disease:
- The usual age of onset is between 20-30 years of age. But it can occur in older ages up to 70 years.
- Abdominal pain and bloating.
- Constant diarrhea.
- Diarrhea can also be intermittent or not present. Constipation can also occur.
- Nausea and vomiting.
- Weight loss.
- Easy fatigue and iron deficiency anemia.
- Itchy, blistery skin.
- Osteoporosis and osteomalacia (body aches).
Celiac disease is diagnosed by a blood test or by taking a small intestine biopsy.
Call your doctor if you suspect celiac disease. Learn more.
5- Inflammatory bowel disease.
Inflammatory bowel disease refers to 2 major conditions:
- Crohn’s disease: Unexplained inflammation and ulceration at any part of your gut (from the mouth to the anus).
- Ulcerative colitis: Unexplained inflammation and ulceration affecting the large intestine only (the colon and the rectum).
According to the CDC, about 1.8 million U.S adults (0.9%) had inflammatory bowel disease,
Symptoms of IBD:
- Persistent or recurrent diarrhea.
- Abdominal pain.
- Blood or blood and mucus coming out with or without a stool.
- Weight loss.
- Generalized fatigue.
- Fever may occur.
- Loss of appetite.
Suspect IBD if you have a prolonged history of abdominal pain, mucus, constant diarrhea, and blood in stool without obvious cause.
The main differences between Crohn’s and ulcerative colitis are summarized in the below table.
| Type | Crohn’s Disease | Ulcerative Colitis |
| 1- Site | Any part of the GI tract (from the mouth to the anus) | The colon and rectum. |
| 2- Lesions | Deeper, it can involve all the layers of the GI wall. | Usually superficial (only in the innermost layer) |
| 3-Predominant symptom | Crampy abdominal pain | Bloody diarrhea. (can be constant) |
| 4- Complications | Fistulas, abscess, intestinal obstruction | hemorrhagic toxic megacolon. |
| 5- Risk of colon cancer | Slight increase | Marked increase |
Ulcerative colitis and Crohn’s disease are major diseases that require medical care and follow-up.
If you have a long history of recurrent abdominal pain, constant diarrhea with blood, and mucus in stool, consult your doctor.
MORE:
- Constant Diarrhea & Abdominal Pain: 8 Causes Simplified.
- Why is your Stool Never Solid anymore? 7 Causes of Chronic Loose Stool.
- 7 Causes of Constant Loose Stool every day.
6- Medications.
Vague constant diarrhea for long periods can result from medications you take. Diarrhea is a documented side effect of over 700 medications (reference).
Common medications that can cause constant diarrhea:
- Antibiotics: Any antibiotic can kill the beneficial bacteria inside your colon.
- Some anti-diabetes medications: Metformin and gliptins (vildagliptin, sitagliptin, and others), can cause diarrhea and stomach gurgling.
- Laxative overuse.
- Stomach/GERD medications: PPIs (as omeprazole, esomeprazole, and pantoprazole) and H2 blocker inhibit stomach acid. This inhibition will allow for the overgrowth of bacteria inside the small intestine and colon, causing stomach gurgling and diarrhea.
- Others, such as chemotherapy and immunosuppressive medications, can also cause such conditions.
The complete list of medications causing diarrhea is HERE and HERE.
7- Colorectal cancer.
Abdominal pain alone is a rare presentation of colon cancer. Isolated abdominal pain presents in only 3.8% of colon cancer patients (reference).
A change in bowel habits (such as constant diarrhea) is the most frequent sign of colon cancer.
The recent onset of prolonged constant diarrhea in older ages is suspicious of colorectal cancer, particularly in those with multiple risk factors.
Risk factors for colorectal cancer include:
- Age (especially those who are older than 45 years.
- Family history of colorectal cancer.
- A diet high in fats and processed meats. A low-fiber diet is also a major risk factor.
- Smoking and alcohol abuse.
- Obesity.
- Physical inactivity and sedentary lifestyle.
- Diabetes mellitus.
- IBD.
- African American Race.
Learn more about the risk factors of CRC.
Symptoms of colorectal cancer (with frequency):
- Change in bowel habits (Unexplained diarrhea or constipation): in 75% of patients with colon cancer.
- Blood in the stool (dark or bright red): 50%.
- A sense of rectal mass: in 25%.
- Anemia (iron deficiency): in 10%.
- Isolated abdominal pain: only 3.8% of cases.
- Other symptoms such as weight loss, unexplained fever, nausea, and anorexia are also present.
Learn more:
Can yellow stool be a sign of colon cancer?
It is IBS or colon cancer, differences explained.
7- Recurrent or persistent infections of the gut.
Recurrent or persistent infections can lead to constant diarrhea. The most common persistent infections that can cause constant diarrhea are (reference):
- Closteroides difficile.
- Aeromonas.
- Giardia.
- Amebae.
- Campylobacter.
- Cryptosporidium.
- Cyclospora.
- Whipple’s disease.
This form of diarrhea is usually severe watery, and constant diarrhea for years. It may lead to complications such as malabsorption and weight loss.
Chronic infectious diarrhea is more common in people with weak immune systems. Examples are patients receiving chemotherapy, immunosuppressive medications, and people with HIV.
Your doctor usually needs to do a stool culture or take an aspirate from the small intestine or the colon to detect the causative organism.
More: instant diarrhea after drinking water
8- Overflow diarrhea.
Overflow diarrhea occurs in people with constant severe constipation or stool impaction. Liquid stool leaks from around the rectum’s hard stool, causing diarrhea.
This “overflow” or “paradoxical” diarrhea can be constant and prolonged. Patients with overflow diarrhea may experience a constant sense of mass in the rectum.
They also may suffer from a sense of incomplete evacuation due to the hard stools in the rectum.
9- Others (less frequent or rare).
The causes of constant diarrhea are numerous. No room in this article to explain every cause. Click on the topics below to learn more about each condition (reference).
Infrequent causes of constant (chronic diarrhea):
1. Small bowel bacterial overgrowth
3. Lymphoma
4. Surgical causes (e.g., small bowel resections, fecal incontinence, internal fistula)
9. Diabetes
12. Cystic fibrosis.
Rare causes of constant (chronic) diarrhea:
1. Rare small intestinal diseases (e.g., Whipple’s disease, tropical sprue, amyloid, intestinal lymphangiectasia)
2. Hypoparathyroidism
3. Addison’s disease
4. Hormone-secreting tumors (VIPoma, gastrinoma, carcinoid)
5. Autonomic neuropathy
6. Factitious diarrhea
7. Brainerd diarrhea (possible infectious cause not identified)
- Evidence-based
- Written by a doctor.

Related Posts:
- Unexplained Diarrhea & No Other Symptoms: 9 Common Causes.
- Top 9 Mistakes That Make Your IBS in Constant Flare-Ups.
- Yellow Watery Stool: Common Causes And Treatments.
- Yellow diarrhea: 12 Causes, Doctor Explains.
- Can Stress Cause Appendicitis? Gastroenterologist Explains.
- Untreated Pancreatitis: 6 Possible Scenarios…